The need for better diagnostic tools
In current clinical practice, the gold standard for psoriasis assessment is clinical scoring – i.e., qualitative assessment by the physician, usually through a visual examination. In particular, the psoriasis severity index (PASI) is the most widely used measurement tool for psoriasis.
This approach has significant disadvantages: it is subjective, provides only superficial assessment, is insensitive to subtle disease changes, and provides no information on pathological features. Beyond the PASI score and similar clinical scores, imaging methods such as optical coherence tomography, high frequency ultrasound, and laser Doppler imaging have been explored, but so far none have proven robust enough to see wide adoption in clinical practice. While dermoscopy is used most commonly in clinical routine, it can only provide superficial information and does not offer insight into pathological changes at depth in the skin. Thus, there is an unmet clinical need for better methods to assess psoriasis disease status and treatment response.
Raster-scanning optoacoustic mesoscopy (RSOM) is a novel, non-invasive, high-resolution imaging platform that utilizes the photoacoustic effect to visualize the concentration and distribution of naturally occurring chromophores inside the body, such as hemoglobin. Through sampling of optoacoustic signals at high frequency, RSOM offers high resolution (10-40 µm) optoacoustic imaging up to an imaging depth of >1 mm. Results from previous studies have indicated that RSOM may be a valuable new tool to provide quantification of vascular changes in the skin associated with a variety of diseases, such as psoriasis, diabetes, and eczema. Notably, RSOM has shown the potential to perform better than established techniques and diagnostic tools, especially when quantitative and timely assessment is needed.
![]()
Precise disease monitoring with RSOM
In a recent study published in Science Translational Medicine, researchers at the Technical University of Munich further examined the ability of RSOM to monitor patient response to psoriasis treatment. Here, they performed longitudinal measurements on 19 patients with plaque psoriasis undergoing various treatments to manage disease symptoms. Skin plaques were evaluated using RSOM imaging as well as the clinical gold standard method of PASI scoring, with a focus on assessing the relative performance of each method to report changes in psoriasis severity and treatment response.
Using RSOM, the skin microvasculature could be visualized in high resolution. Moreover, RSOM revealed striking differences in morphological features between psoriatic and healthy skin, which were corroborated by histological analyses of the same tissue areas.
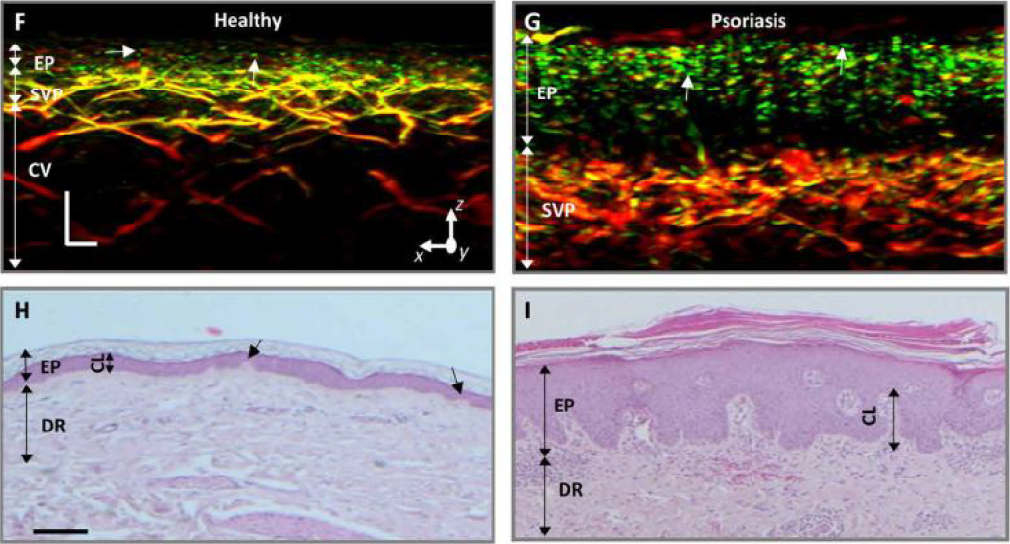
Cross-sectional RSOM and histological images of healthy and psoriatic skin.
To assess the ability of RSOM to detect changes in skin morphology relating to psoriasis treatment response, the same psoriatic plaques in fourteen patients were monitored over ten days of treatment with conventional therapy (i.e., daily application of standard topical treatments and simultaneous phototherapy). The plaques were inspected visually and scored with PASI as the gold standard assessment method. In addition, the plaques were evaluated in detail with RSOM, with several metrics of skin microvasculature derived from the datasets.
While the downward trend of the RSOM-derived metrics correlates well with the downward trend of the PASI score, RSOM also appeared to be able to detect ongoing changes in skin morphology as a result of therapy which were not captured by the PASI score. Notably, while the PASI score in the exemplary case remained unchanged between days 8 and 10 of treatment, qualitative evaluation of RSOM images as well as the RSOM-derived metrics indicate ongoing skin recovery during the same period.
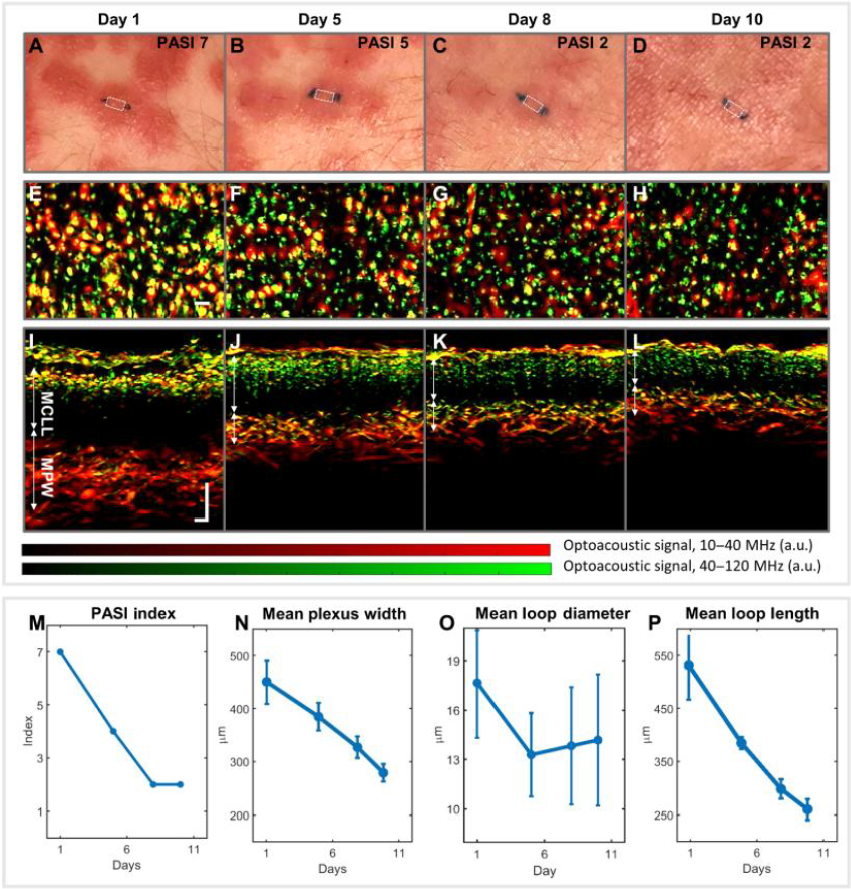
Assessment of the same psoriatic plaque over ten days of treatment with conventional therapy. (A-L) Clinical photographs, coronal RSOM images, and cross-sectional RSOM images. (M-P) Change over time in PASI score and three RSOM-derived metrics of skin microvasculature.
These findings were also observed in the case of patients undergoing therapy with biologics. For example, there were cases where scoring with PASI indicated that the psoriatic skin was fully healed, while RSOM imaging and RSOM-derived metrics of skin microvasculature indicated residual psoriatic pathology and ongoing skin recovery.
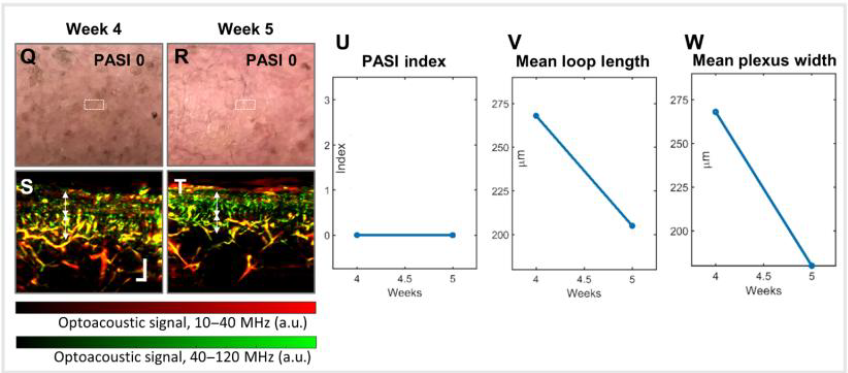
Assessment of psoriatic skin of a patient undergoing biologics treatment. (Q and R) Clinical imaging and (S and T) RSOM imaging of affected skin. (U-W) Local PASI score and two RSOM-derived metrics of skin microvasculature.
Similar to the PASI score, the authors propose an RSOM-derived scoring method to monitor psoriasis status and treatment response. This new, objective score would combine the two most prominently affected RSOM-derived metrics of skin microvasculature explored in this study. When compared to the corresponding local PASI score, it showed good correlation while also capturing changes in skin morphology that were not reflected in PASI scores. Thus, this RSOM-derived scoring system could offer a more objective means to assess psoriasis status over time.
![]()