Non-invasive functional imaging is central to monitoring the development and progression of ischemic lesions over time to aid the understanding of the process and potential impact of therapeutic intervention. MSOT can easily assess the changes in local blood oxygenation and vascular perfusion associated with such events through the intact skin and skull in rodent models, thereby providing an ideal non-invasive approach to monitor the impact of such events.
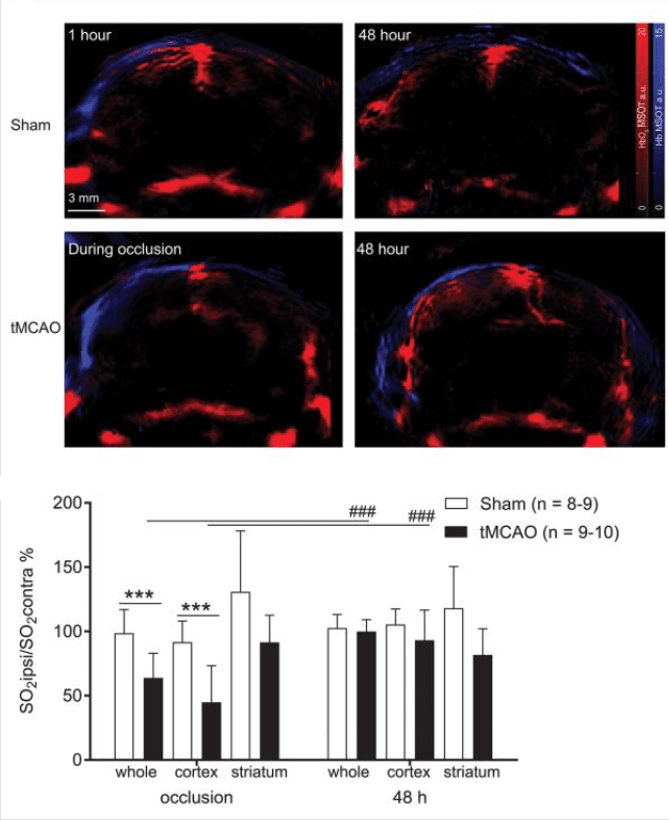
Oxy- and deoxy-hemoglobin shown in red and blue, respectively, in sham or tMCAO mice during or 48 hours following the surgical procedure. Oxygen saturation was calculated in multiple brain regions at both time points.
To assess the influence of transient middle cerebral artery occlusion (tMCAO) on brain regional tissue oxygenation, HbO2∕Hb levels in the brain of tMCAO and sham-operated mice were measured noninvasively in vivo during occlusion and at 48 hours after reperfusion using MSOT to calculate brain tissue oxygen saturation, SO2. Lower SO2ipsi∕ SO2contra ratios were detected in the lesion of tMCAO compared with sham-operated mice and in the cortical lesion, indicating severe focal ischemia.
Ni et al. Neurophotonics. 2018
In combination with real time operation and high spatial resolution in deep living tissues, the intrinsic sensitivity of MSOT to functional blood parameters may see it become a valuable and unique tool in the development and monitoring of treatments aimed at suspending the spread of an infarct area.
Kneipp et al. Photoacoustics. 2018
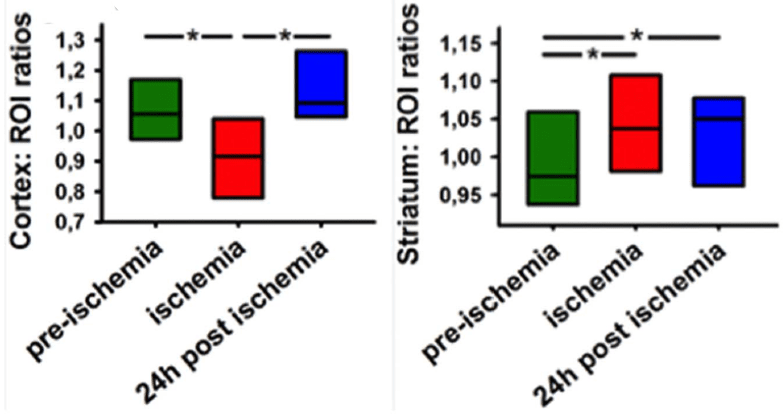
Ratios between the lesion caused by the stroke and the contralateral brain region, either the cortex or the striatum, were quantified before, during, and 24 hours post-occlusion.