Neuromuscular diseases (NMDs) such as Duchenne muscular dystrophy (DMD) and spinal muscular atrophy (SMA) lead to the loss of muscle function and eventually to death. Current diagnostic methods rely on subjective physiological examinations such as the six-minute walk test (6-MWT). With promising yet extremely expensive therapeutics coming to market, an objective method of assessing disease status is critical. MSOT has shown the potential to be such a method, by quantifying the collagen concentration in muscle tissue as a biomarker of tissue degeneration.
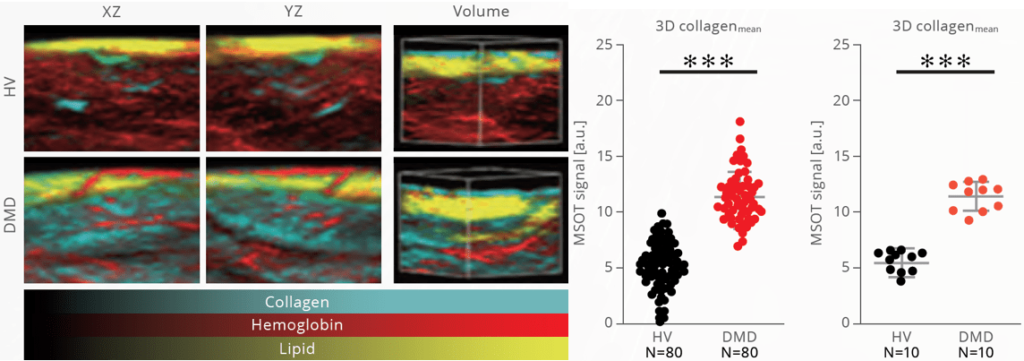
Representative MSOT images from DMD patients and healthy volunteers (HV), visualizing collagen (cyan), hemoglobin (red), and lipids (yellow). MSOT signals were quantified per region scanned, or on a per-patient basis.
Ambulatory DMD patients aged 3 to 10 years and age-matched healthy volunteers were enrolled in a pilot study to evaluate MSOT performance to assess neuromuscular disease in humans. MSOT measurements revealed increased collagen (reflective of fibrosis) in the muscle tissue of DMD patients compared to healthy volunteers.
Regensburger et al. Nat Med. 2019
The results from the pilot study demonstrate the excellent diagnostic performance of MSOT imaging to distinguish healthy from diseased muscular tissue. Moreover, MSOT signals were significantly correlated to standard physiological and functional tests like the 6-minute walk test (6MWT). These results suggest that MSOT imaging might fill the urgent need for an easy and objective assessment of DMD disease progression and could be evaluated for treatment monitoring in future clinical studies.
Regensburger et al. Nat Med. 2019
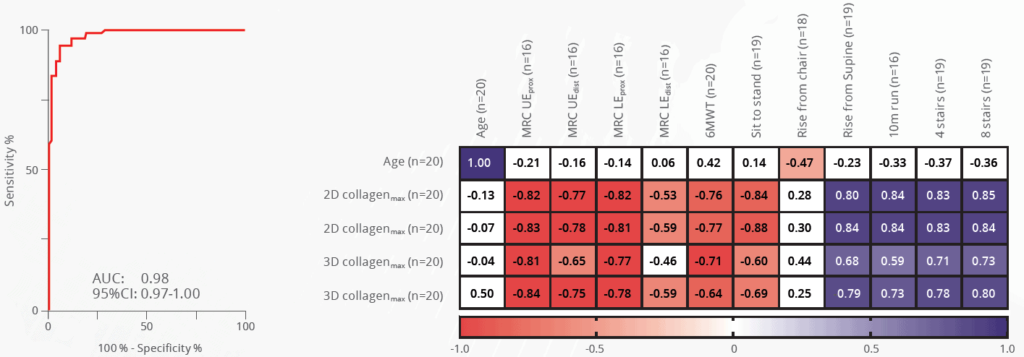
A Receiver operator characteristic curve shows the performance of MSOT, while negative (red) and positive (blue) correlations with clinical gold standard assessments are shown in a table.
MSOT has also demonstrated the ability to assess neuromuscular diseases in a second disease, Spinal Muscular Atrophy (SMA). In a pilot study, SMA patients (age 9.0 ± 3.7 years) and age-matched healthy volunteers (age 8.7 ± 4.3 years) were scanned with MSOT, and the results were compared with functional tests such as the Expanded Hammersmith Functional Motor Scale (HFMSE) and Revised Upper Limb Module (RULM). Not only did MSOT results correlate well with clinical gold-standard functional assessment, MSOT images also showed patchy scattered patterns comparable to a moth-eaten appearance. Such morphological changes could also be detected by the ultrasound module on the MSOT Acuity Echo system (Reflection-mode Ultrasound Computed Tomography: RUCT). Interestingly, when compared to standard clinical B-mode ultrasound, RUCT showed better performance. In the future, combining optoacoustic imaging and RUCT could potentially further improve the diagnostic accuracy of MSOT for neuromuscular diseases.
Regensburger et al. Photoacoustics. 2022
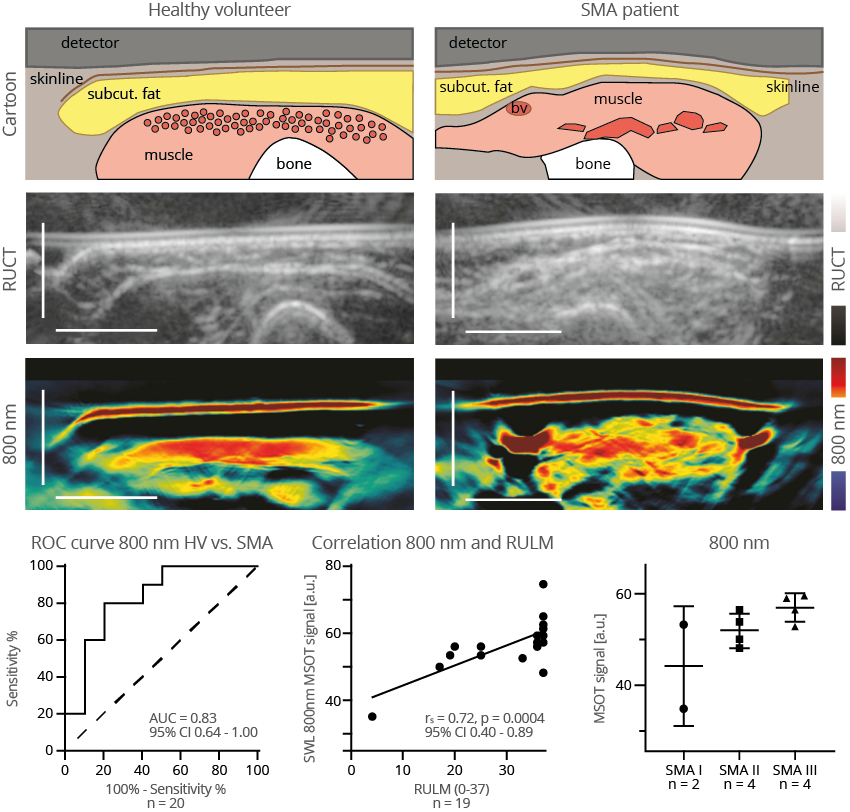
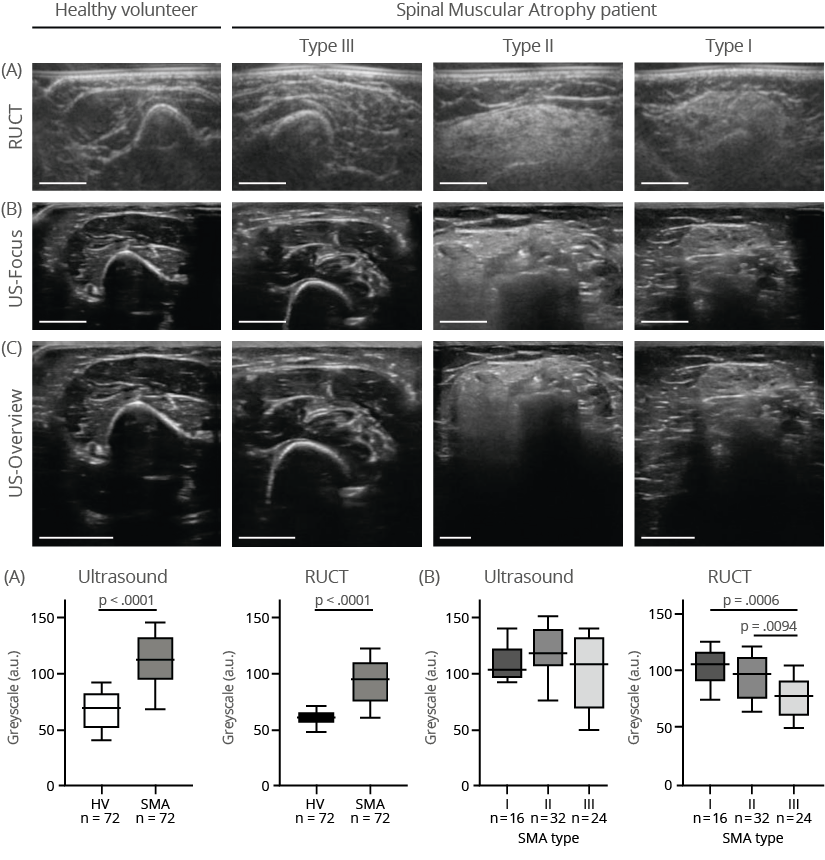
Multimodal MSOT imaging comparison of healthy versus SMA-affected muscles, highlighting structural and compositional differences. Muscle tissue from the SMA patient shows patchy hypertrophic and atrophic fibers as well as increased echogenicity, in contrast to the uniformity of healthy muscle.