Melanoma is the fastest growing and fifth most common cancer. The standard for diagnosing and staging melanoma is a biopsy of the primary tumor followed by surgical removal and histological assessment of the sentinel lymph nodes (SLNs). Detection of SLNs is performed via lymphoscintigraphy, following injection of the radioactive compound Technetium (99mTc). The diagnostic work-up is therefore highly invasive and exposes the patient to ionizing radiation. Initial clinical trials show that MSOT has the potential to be a non-invasive and radiation-free alternative for primary lesion characterization, SLN detection, and assessment of metastatic involvement of SLNs.
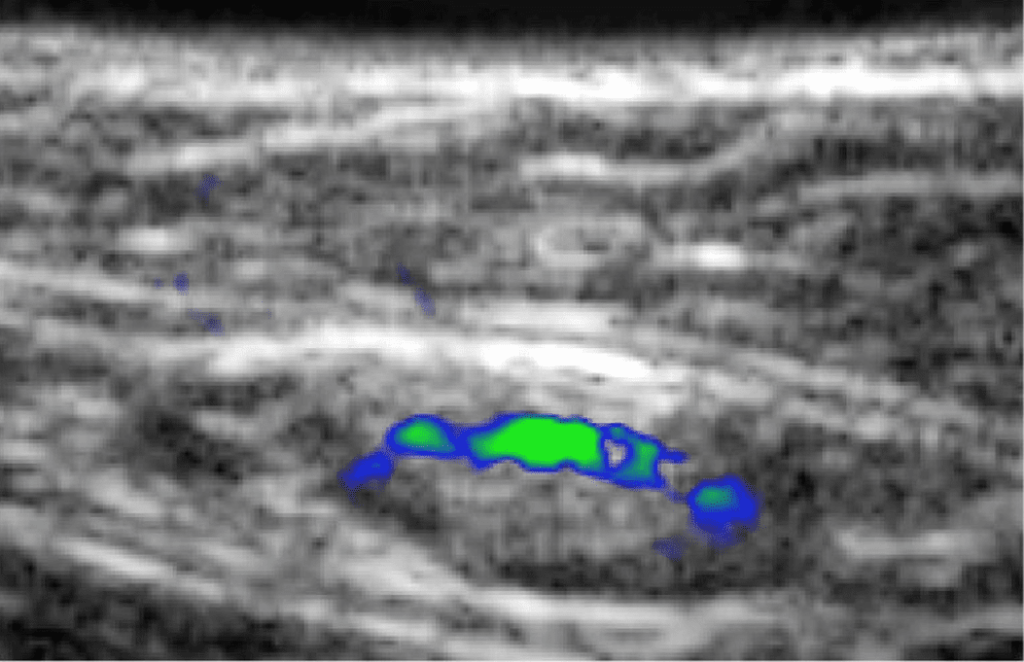
B-mode ultrasound image with an overlay of spectrally unmixed ICG MSOT signal, showing the location of the sentinel lymph node.
A recent clinical study showed that MSOT has the potential to improve melanoma diagnosis. The dye indocyanine green (ICG) is injected peritumorally to identify the sentinel lymph node (SLN), overcoming the need for radioactive 99mTc. MSOT was shown to identify the presence of ICG in SLNs at several centimeters depth.
Stoffels et al. Sci Transl Med. 2015
Following ICG-based SLN detection, MSOT has been used to non-invasively determine the nodal status and rule out the presence of metastases based on the detection of melanin in the SLN. The absence of melanin in the SLN effectively ruled out a metastasis, which could potentially spare the patient from surgical SLN extirpation.
Stoffels et al. Sci Transl Med. 2015